Scoliosis is a deformity of the axis of the spine in the frontal, sagittal and horizontal planes. It mainly affects children and adolescents, but can also occur in adults, sometimes due to a disease or the existence of malformations. Scoliosis is twice as common in girls as in boys. It can be observed at any age but is much more common at the age of more than 10 years. It is hereditary, so people with scoliosis are very likely to pass it on to their children, in any case, there is no correlation between the severity of scoliosis from one generation to the next.
CONTENT:
What are the causes?
Scoliosis is a condition that leads to the curvature of the spine. It can affect any part of the spine, but especially the thoracic area (thoracic scoliosis) and the lower back (lumbar scoliosis). Most of the time, the causes of the change in the shape of the spine are not known, but doctors believe that it has to do with:
- Some neuro-muscular disorders – these affect the muscles and nerves and include polio, muscular dystrophy and cerebral palsy;
- Some genes – it is believed that there is at least one gene involved in the transmission of scoliosis;
- Leg length – a person who has one leg longer than another can develop scoliosis;
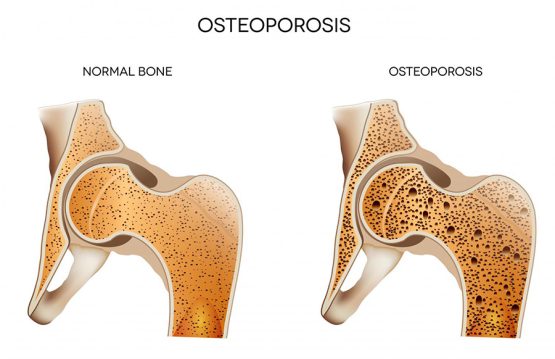
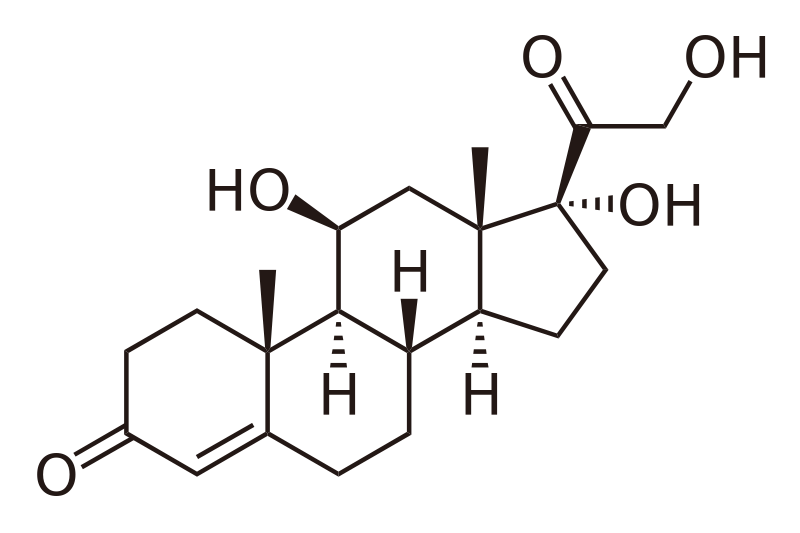
- Osteoporosis – scoliosis can occur as an effect of this disease, once bone degeneration affects other areas of the body, so the spine;
- Incorrect posture – at the office or inappropriate wearing of the backpack.
What are the symptoms?
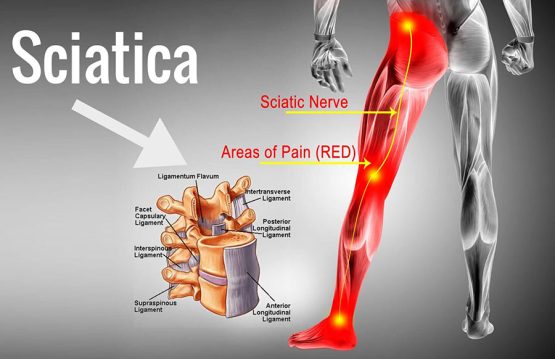
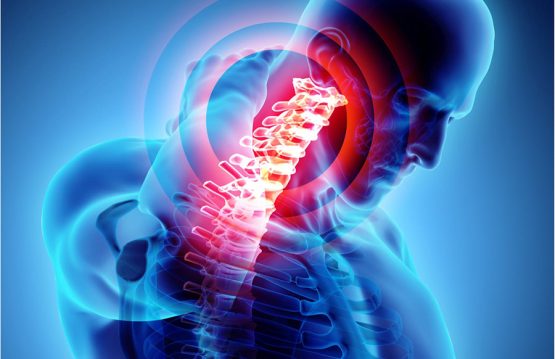
Often, the symptoms are noticed especially by those around. Once the spine grows, it pushes the shoulders and hips so that they can look asymmetrical. Most of the time, scoliosis does not affect movement and does not cause consistent back pain until the curvature becomes severe. Sometimes, unexplained back pain can occur because the curvature of the spine puts pressure on the spinal nerves and sometimes on the entire spinal cord. In addition to mild pain, at least at first, weakness, numbness, and pain in the lower extremities may occur. Another indication of scoliosis is the feeling of fatigue, after long periods of sitting or standing. As the spine becomes more deformed, the muscles must make an extra effort to keep the body aligned. Over time and in the absence of treatment, scoliosis progresses and puts pressure on the chest cavity, restricting the person’s ability to breathe easily and widely.
What is the treatment?
Most adolescents who have a type of disease that does not have a clear cause are monitored at regular intervals (every 6 months). The corset The corset is the standard treatment for teenagers who have a spinal curvature between 25 and 40 degrees. The purpose is stiffening and temporary correction. Surgery Those who have a spine curve between 40 and 50 degrees should consider surgery. The doctor’s goal is to make sure that curvature does not get worse. However, the operation does not completely straighten the spine. During the procedure, metal implants are used to correct the curvature and to maintain a correct position until a bone graft is placed. Surgery for scoliosis involves joining the vertebrae, a process called spinal fusion. Many studies have shown that electrical stimulation and exercise programs cannot prevent the progression of scoliosis. However, people affected by this disease must remain active.